What to expect at your first Pelvic Floor Physical Therapy appointment
This is where YOUR story is finally heard

Every initial evaluation commences with a conversation. I always introduce patients to "the club," a private treatment room designated for my pelvic floor caseload. This room is meticulously designed to maintain a calm, inviting, and private atmosphere, ensuring privacy and security during treatment.
I initiate the process by delving into the patient’s history of symptoms and related background. Subsequently, I conduct an assessment of the lower back, hips, and pelvic floor muscles to evaluate their strength, function, tone, flexibility, and tissue tension. I keenly observe movement patterns and how the patient bears weight—crucial indicators of the body's efficient utilization of strength.
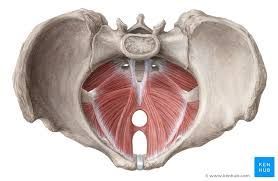
For patients deemed suitable, an external and internal pelvic floor examination is performed. The pelvic floor refers to a group of muscles, ligaments, and connective tissues that form a supportive hammock-like structure at the base of the pelvis. It spans the area between the pubic bone at the front of the pelvis and the tailbone at the back. To illustrate, just as a physical therapist would palpate the muscles around the head, neck, and shoulders when addressing headaches, a pelvic floor exam serves a similar purpose. The patient's consent for assessment and treatment is of utmost priority, with the option to decline at any juncture.
Treatment encompasses interventions and education pertaining to strengthening, bowel and bladder health, vaginal and uterine health, sexual well-being, as well as techniques for optimal breathing and mechanics during daily activities.
Though it may be tempting to attribute pelvic dysfunction to a natural part of the aging process, the reality is different. While it's true that one in three women will experience pelvic floor dysfunction, its prevalence does increase with age. Nonetheless, most cases of dysfunction respond well to treatment. Rather than dismissing your symptoms, take the step to discover your "club" today!